In Brief
Electronic health records (EHRs) were supposed to bring connection and clarity to healthcare — a single, elegant system for coordinating treatment, reducing errors, and saving time. Instead, for many therapists, they’ve come to symbolize the opposite: another invisible labor, another layer between them and their clients.
And this isn’t a design flaw. It’s a design choice. Most EHRs were built for medicine — prioritizing billing codes and checkboxes over narrative nuance and clinical reasoning. They reflect the priorities of the institutions that funded and incentivized them: large hospitals, insurers, and policymakers who saw digitization as an economic and administrative tool, not a clinical one. In short, while the EHR may be indispensable, it’s also a mirror of the system’s most persistent imbalance: more time spent managing care than delivering it.
When behavioral health finally joined the digital era, it did so as an afterthought — excluded from most federal funding and left to retrofit systems built for someone else’s workflow. Today, the EHR is indispensable to running a practice. But it’s also a daily reminder of how mental health care was sidelined in the evolution of healthcare technology — forced to adapt to systems that were never designed to serve it.
The First EHRs
For much of the 20th century, therapists worked in a deeply analog world. Client records lived in manila folders, tucked behind locked filing cabinets, accessible only to the clinician who wrote them. These records were messy, human, and profoundly local, but they were also fragmented. Coordination with physicians or hospitals was rare, and if a client’s file needed to travel, it often did so by fax.
The earliest digital medical record systems emerged not from private practices but from defense contracts and hospital experiments. In the 1960s, the Lockheed Corporation (now Lockheed Martin) designed one of the first “clinical health information systems,” a project so expensive and complex that only major institutions like the Mayo Clinic could participate. Around the same time, Dr. Lawrence Weed introduced the Problem-Oriented Medical Record (POMR), which organized patient data by diagnosis rather than by visit. This framework would later shape the logic of every major EHR: data categorized, structured, and ready for billing.
By the 1970s, the U.S. Veterans Administration built on that foundation with the Decentralized Hospital Computer Program, the ancestor of today’s VistA system. It was efficient, integrated, and revolutionary for large-scale care. But its standardized entries, coded problems, and physician-oriented workflows reflected the priorities of medicine, not mental health.
Therapists, especially those in solo or small-group practices, were left on the periphery. Their tools remained pens and paper, their infrastructure self-financed, their work seen as peripheral to the great modernization of healthcare.
Digitization Arrives, and Insurers Take the Lead
By the 1990s, the shift toward digital recordkeeping was no longer optional. Hospitals and insurers needed standardized, coded data to process the growing volume of claims and comply with new privacy laws. HIPAA, passed in 1996, accelerated this transformation — not by mandating electronic health records, but by standardizing electronic transactions.
HIPAA was less about helping clinicians document care and more about helping insurers process payments safely and consistently. That distinction matters: it meant that from the start, the EHR was financially motivated. Systems were built to produce compliant billing codes and auditable records, not to capture therapeutic nuance or human complexity.
By the early 2000s, as the internet matured, hospitals began investing heavily in digital infrastructure. Therapists, however, remained largely outside that conversation. The cost of EHRs was prohibitive, and there were few behavioral health–specific options. For many, it was still cheaper and simpler to stay on paper. That would soon change, though not in their favor.

The Incentive Gap: When Mental Health Was Left Behind
In 2004, the federal government created the Office of the National Coordinator for Health Information Technology (ONC) to push for universal adoption of EHRs. The big push came five years later with the HITECH Act of 2009, which poured approximately $25.9 billion into health IT adoption. Through the “Meaningful Use” program, hospitals and other eligible organizations could earn tens of thousands of dollars per provider in federal incentives by implementing certified EHR systems and meeting specific usage criteria.
But behavioral health providers were deliberately excluded from most of these federal incentive programs.
Psychologists, licensed professional counselors, marriage and family therapists, and most social workers were not considered “eligible providers” under Medicare and Medicaid EHR incentive programs: a bureaucratic distinction that had profound consequences.
By 2015, 96% of hospitals had adopted certified EHRs, according to a 2016 report released by the Office of the Assistant Secretary for Technology Policy. Behavioral health lagged far behind.
That gap wasn’t just about technology, it was about value. While other medical specialties were given resources, training, and subsidies to modernize, therapists were expected to self-fund and self-teach. The message was clear: your work matters, but not enough to invest in.
Systems Built for Billing, Not for Care
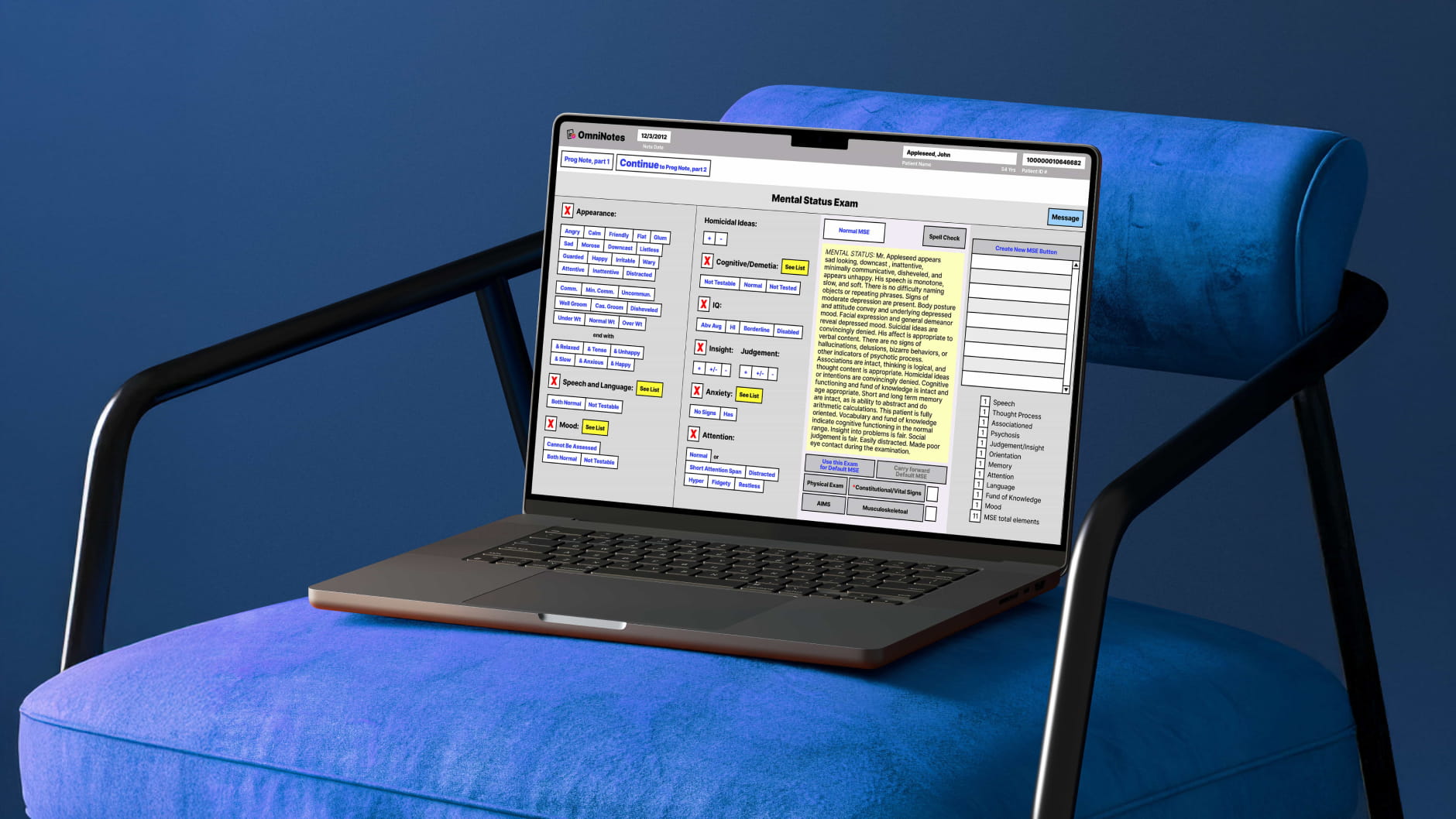
When mental health providers finally began adopting EHRs en masse in the mid-2010s, what they found waiting for them were systems built for billing departments. The templates, prompts, and dropdowns assumed a medical model: diagnosis-driven, problem-oriented, code-based.
This isn’t just a surface-level issue, it’s structural. EHRs were never optimized for psychotherapy’s unique documentation needs: progress notes that blend clinical reasoning, relational context, and subjective experience. Instead, they demanded conformity to insurer expectations, medical necessity, standardized interventions.
As a result, clinicians have learned to accommodate the EHR instead of the other way around: reshaping their language, documentation practices, timing, and even thinking to fit a platform that was never really designed for them.
The Features and Limits of Legacy EHRs
The exclusion from federal incentives didn’t just slow adoption; it reshaped the entire EHR marketplace for mental health. Without subsidies, large medical vendors like Epic and Oracle Health focused on hospitals and physician groups, leaving smaller behavioral health practices to navigate a patchwork of niche platforms.
Many of these legacy mental health EHRs evolved from billing software, layering on clinical features over time. The result: clunky interfaces, rigid templates, and slow workflows that force therapists to click through dozens of screens to do basic tasks.
A 2022 study in the Journal of Medical Internet Research found that 73% of clinicians working in a psychiatric hospital raised the issue of workflow in connection with reduced efficiency, specifically, the challenge of balancing service user care needs and using the EMR. Workflow misalignments led to less time for direct care, which was viewed as affecting the therapeutic relationship. (Kariotis et al., 2022).
Even now, therapists pay a premium for systems that barely fit their needs. Consider the numbers: SimplePractice raised its base plan, which does not include basic benefits like scheduling reminders, from $39 to $49 per month in 2024. Therapy Notes announced they are raising their solo plan from $59 to $69 per month starting in December 2025. As of November 2025, AI note-taking tools like Freed can cost about $90 per clinician each month, and JoyPsych $149 every month.
These legacy EHRs can easily exceed $5,000-$7,000 annually, once add-ons like telehealth, AI note-taking, and analytics are included. What’s more is that these expenditures are entirely out-of-pocket for providers who were never funded to digitize in the first place.

What We Lost in Translation
Every technological revolution creates winners and losers. For EHRs, the winners were the insurers, administrators, and regulators who gained access to structured, billable data. The losers were the clinicians whose work became data entry.
Therapists entered the EHR era not because it made their care better, but because compliance demanded it. Each dropdown menu, each diagnostic code, each “required field” represents a shift in what counts as legitimate documentation. Notes once meant to capture human change now function primarily to justify reimbursement.
It’s not that therapists resist modernization. Rather, it’s that the modernization they were offered never centered their work. Behavioral health wasn’t given the same investment, design input, or policy support as medicine. It was told to keep up, but not invited to lead.
A Therapist-Centered Future
But the story isn’t entirely bleak. New, therapist-centered systems are emerging that aim to reverse this prevailing hierarchy by emphasizing usability, narrative flexibility, and integration.
This new era of practice support systems recognize the emotional and cognitive load of therapy itself. And perhaps more importantly, smarter EHRs can begin to feel like a tool that respects the therapist’s labor, rather than one that undermines it. Features such as template suggestions, paperless intakes, and pre-filled insurance forms are designed to reduce cognitive friction, leaving clinicians able to focus on nuance, empathy, and connection. This is a subtle but profound shift: for the first time, the technology is working for the therapist, not just for the benefit of insurance systems.
The rise of AI and therapist-centered design reflects a broader recognition: digital tools must be flexible, adaptable, and responsive to human patterns of clinical reasoning, not just to billing compliance.
Because the real measure of a record system isn’t how fast it processes claims. It’s whether it gives therapists back the time and presence they need to do their best work.
If you'd like a more in-depth look at the history and future of EHRs, please check out Behavioral Health EHRs: What's Working, What's Broken, What's Next.

How Blueprint can help streamline your workflow
Blueprint is a HIPAA-compliant AI Assistant built with therapists, for the way therapists work. Trusted by over 50,000 clinicians, Blueprint automates progress notes, drafts smart treatment plans, and surfaces actionable insights before, during, and after every client session. That means saving about 5-10 hours each week — so you have more time to focus on what matters most to you.
Try your first five sessions of Blueprint for free. No credit card required, with a 60-day money-back guarantee.























